Lunula laser Webinar – Case Studies Discussions
October 24th, 2018
If you’re using the Lunula cold laser in your practice or are wanting to learn more about the real results we’re seeing with the laser, then this article is exactly for you. Last month, we had the absolute pleasure of speaking LIVE with Lunula expert, Martine Abrahams. Together with all those that tuned in, we examined case studies, talked about her processes, tips, tricks and had her answer all your questions! For those that were unable to make the webinar, here are the KEY points and messages that you can start implementing in your practice today.
Introducing: Martine Abrahams
Alongside being a fantastic Podiatrist with over 22 years of experience, Martine was also the first to pioneer both the Pinpointe (hot) laser in the UK, and then the Lunula (cold) laser after its global release. Initially, she did this because she recognised that laser was the superior treatment solution to a very frustrating problem among patients and Podiatrists alike. Her decision to switch to the Lunula laser was more than simply eliminating pain for patients, it was to provide the most effective treatment available that is also less time consuming, easy to administer, and with no risk of complications.
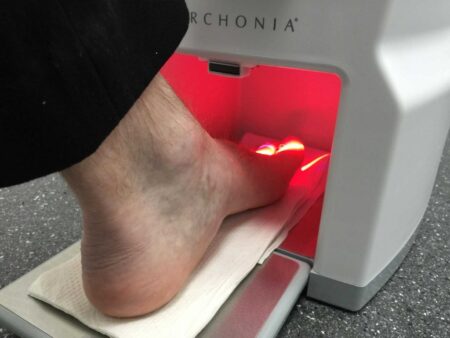
Introducing: Lunula Cold Laser
For those that aren’t familiar with the Lunula, this laser uses two cold beams, set at frequencies of 405nm and 635nm respectively. The 405nm beam damages the fungus itself and helps the body break down the fungus by producing hydrogen peroxide which is an antiseptic and antimicrobial. The 635nm beam stimulates the immune system and causes vasodilation by producing nitric oxide. This allows improved blood flow at the feet and encourages the immune system to start healing and regeneration.

Recommended Treatment Times
During her years with the Lunula, Martine has trialled various treatment protocols including daily treatments, monthly treatments, doubling and halving treatment times, and more. What she has found to be most effective is administering four treatments at intervals of no more than four weeks apart – ideally weekly or fortnightly.
Martine then has monthly reviews for the first six months before increasing the review timeframe to every six to eight weeks. These reviews are not charged (if no debridement or further treatment is needed) and she offers these reviews digitally if patients prefer, whereby a photo of the nails is sent to her for review. For very mild infections, Martine notes that just two treatment sessions may suffice.
Lunula Is Not Just for Fungal Infections
What may come as a surprise for many practitioners is that Martine uses the Lunula successfully for much more than just fungal nail infections. Because of the function of the 635nm beam in the healing and repair process, it is also able to help with psoriasis, traumatic nail changes from damage, friction from footwear and more. Martine reports improvement in the appearance of the nails in almost 100% of her patients, with or without fungal nail infections. Given that the primary frustration for patients is the appearance of the nail, we think it’s fantastic that the Lunula can provide an answer for this too.
The 8 Webinar Tips To Start Using Today
Here are eight of the tips that Martine shared throughout the webinar. These come from her experience and you can start adopting them today. To listen to the case studies associated with these tips, please listen to the full webinar.
#1: Debride Aggressively
In Martine’s practice, she always debrides aggressively any nail or section of the nail that isn’t healthy, to produce the best results. When this is done pre-treatment, the laser is most effective, and the healing begins very quickly after treatment. Often, after treatment has finished, any whiteness/ discolouration left on the nail is superficial and can come off when reduced with a drill.
#2: Limit Additional Treatments
Only administer additional treatments if there is definite evidence of a live fungal infection. If the nail has patches of new yellow or white, or is crumbly or loose where it wasn’t before, this is a good sign of a fungal nail infection as the fungus causes the nail plate to come away from the nail bed.
#3: There Is Such a Thing as Over-Treatment
Because there is a maximum amount of blood that can get to the feet and nails, there is a point at which additional treatments stop being useful. While the effects of overtreatment aren’t negative, the body can begin to do the opposite where it says, ‘I’ve done this, I don’t need to keep doing this’ and it stops being useful. This being said, we have seen some over-treatment cause the nails to be flakier and less healthy-looking.
#4: Taking Good Nail Photos
- Make sure the foot is flat! Having the toes scrunched causes whiteness around the joints and redness at the ends which can distort the image
- Remove the superficial markings and discolouration so you (and your patients) can see true progress over time
- Ensure to get monthly photos, whether they’re taken in-clinic or following up with patients to get them sent in
#5: Problem-Solve Irregular Results
If a nail is not progressing as you had expected, get your thinking cap on! Find out their recent history to get to the bottom of what is going on. There’s almost always an answer for everything! Have they:
- Been on holiday?
- Been wearing steel caps?
- Started new medications or been unwell?
Talk through this with the patient and form a plan to overcome the barriers so they can start seeking the results you both want. The biggest factors that affect the nail are stress (usually work- related) which impairs the immune system, alongside pregnancy where the nails may regress and deteriorate.
#6: Incorporate Nail Care into the Regular Routine Just like going to the dentist, we recommend to our patients that they incorporate nail care and appointments to be incorporated into their regular healthcare routine. This allows us to monitor changes and administer nail care as needed for best long-term outcomes.
#7: Always Collect the History Always find out how long your patient has had the problem to better understand what you can expect with regards to their progress and outcomes. Also get their medical history, particularly which medications they’re taking because these can affect outcomes or expectations.
#8: Educate! Helping patients understand how their daily activities are affecting their nails can make a significant impact on their long-term outcomes. A good example is toenail damage from sports like soccer. The patient needs to take steps to avoid nail damage, so we do simple things like covering the nail with padded bandages and completing footwear assessment to ensure the best fit. Consider all of the factors, and not just the impact of the laser treatment.

Podiatrist Questions & Answers
We received a number of questions from Podiatrists watching the webinar about what Martine has spoken about. The questions and her answers are transcribed below:
When you check in on the nail each month, after the initial sessions, do you apply laser treatment on those sessions?
No. The only time I will laser is if I believe there is a fungal infection there. Where the patient has come in and it’s clear there’s no infection and instead there’s damage from something else, we will very rarely administer more than four treatments. However, for those patients that present initially with onychomycosis, I may carry out more treatments if I feel that either the infection hasn’t cleared or there is a new infection, which sometimes happens.
When we see patients where the infection is present right under the proximal nail fold, the chances are that you may have to do another treatment later on. As the nail grows, you then see what’s coming up from the matrix that you couldn’t see beforehand. As a rule, no I don’t carry out extra treatments unless I feel there is a need to. This is assessed by debridement with a drill – if drilling breaks the nail plate easily, you know that there is a live fungus as it lifts the nail plate from the nail bed. Then yes, I’ll carry out another treatment and see them back in a month and do the same if need be – but hopefully not.
Is it useful to give a client a double treatment in one session (24 minutes on each foot per session)?
Absolutely not. We’ve tried it. 12 minutes is the optimum dosage and what tends to happen is if you do a second treatment straight away, you get no extra benefit. If you continue and do more treatments, the body actually stops doing the good that it’s doing because it gets to the point where it doesn’t know what’s going on. You can only get a certain amount of blood supply going down to the toes and you can only get a certain amount of hydrogen peroxide produced by the body before it stops doing it completely. We’ve tried with 6-minute sessions, 18 minutes, and other various times and 12 minutes really is the optimum.
Many ladies have shellac nail polish which stays on for weeks if not months. It’s very difficult to get them to not wear the polish. Do you have any advice on this?
Shellac is one of the biggest causes of nail fungus – it’s really awful for the nails. I’ve seen several people in my clinic that have developed a fungal nail infection from wearing it. What tends to happen is that when the shellac is not applied particularly well, you get moisture trapped beneath. The fungal nail infection can then rapidly spread because you can’t see it as the nail is covered with the shellac. If it’s on the fingernails it’s actually easy to treat and we’ve had some phenomenal results with it, however, patients are advised to generally not to use shellac again.
When people pay for expensive laser treatment, they don’t tend to go back to shellac. We have antifungal nail varnish in a variety of colours in our clinic. We sell these to patients. I don’t have a problem with people using nail varnish, I understand clearly the effects that having a damaged nail has on people psychologically, and by all means put it on. The advice we give is to not leave it on for longer than a week without giving it a good 24 hours before reapplying, always use a base coat, use a varnish that has an antifungal property, and be very careful when going to salons where we don’t know what the hygiene is like. Steer clear or take your own instruments and varnish. Lighter nail varnish is also better than darker nail varnish for two reasons:
- Less staining of the nail
- Lighter polish doesn’t tend to show the lumps and ridges that dark polish does
Is there a test available that confirms the presence of a fungal nail?
Yes, there are various methods. There are standard cultures that you can send off to a lab. There are in-trays where you take a sample, put it on the in-tray, leave it in a cupboard for a couple of weeks where it grows a culture. There is a 5-min test which I haven’t used yet, but if you’re using the Lunula there’s actually no need to find out whether there is a fungus there or not because the device has the two beams. This means that if there is a fungus present, it should take care of it and if not, the 635nm should still heal the damaged area. This is why testing is not as important as it is with the hot laser as it actually heats the nail and can cause uncomfortable symptoms.
You mentioned the nail of a gel nail you use, what is it called?
Wilde-Pedique. It’s German and they have training sessions all around the world, I’m not sure if they have them in Australia. They have silver in some of their gels which acts as an anti-fungal, so I’d use that first on the nail and then I use the natural beige or core pink that blends in with the skin and then the patients can paint those nails. The gel will have sealed the area overlying the nail. The company says you can leave it on for 3 months, but we don’t leave it on for any longer than 6 weeks and you can replace it straight away. We find that for nails that aren’t adhered to the nail bed, the gel tends to push them down too – it’s a really good product.
Would you suggest treating both feet in one session, so it doesn’t pass from one foot to the other? Is there ever a case where you’d only treat one foot?
Yes, I treat only one foot in a lot of cases actually. If someone has come in and there has been no spread of infection (so only one nail infected), then yes we treat only one foot. Fungal infections only spread if there is a way for the fungal infection to get into the nail. What we find is that with one foot, it tends to be bigger than the other, you tend to get damage to that foot on the nails and not on the other, it’d be good to treat both feet but not all patients want both feet treated. We always give out patients an antifungal cream to use after treatment until they finish the tube – I always suggest they put it on both feet anyway and we keep an eye on the non-affected foot throughout the course of treatment. We have different prices for treating both feet versus one foot. Our price for treating both feet is not double the one foot, it’s only slightly more to encourage people to have both feet treated but some people just don’t want to. I don’t believe there is as much cross infection as we originally thought as once people are educated, they’re more careful. If the nails on a foot aren’t damaged and the patient has had a longstanding infection in one foot only then it’s safe to treat just that one foot.
Do you recommend using urea 40% to soften the nail prior to debridement and during debridement?
I don’t use it but know people that do, but I never have done so. I think if you’ve got a decent nail drill and your debridement skills are good then you shouldn’t need to. I use a variety of different sizes and coarseness for the drill, if you use it initially to get the debris off then maybe that will help but I don’t think you should be softening and putting moisture into an area that has fungus present. My answer is that I can’t categorically tell you as I haven’t used it but I know that people do and are happy to.

Do you augment treatment with antifungal sprays, creams or tea-tree oil?
Yes, we use cream. In the UK, you can’t get sprays or liquid sprays that are bigger than a few millilitres so we did use to give out Lamisil sprays, but they only lasted a few days because they’re so tiny. I like sprays because they’re very easy, whereas I don’t like powders because they clog up pores. Because we can’t get decent sizes of the sprays, we give out terbinafine cream and clotrimazole cream. We apply it to the feet after the first treatment, so they see how to apply it. We apply it from the ankle down, all over the foot, between the toes, and rub it in properly. We ask the patient to do it 1-2 times per day. If they don’t have any evidence of tinea pedis, then they can do it just once a day. If they do have tinea pedis, then apply twice daily.
We give both because clotrimazole treats candida and terbinafine treats dermatophytes. Sometimes it’s very obvious what kind of infection it is (dermatophyte are yellow, candida yeast are white), but other times you really can’t tell especially if it’s a long standing infection.
How do you recommend Lunula laser to your patients? What is your spiel?
I’ve been a podiatrist for a long time, so I can categorically say that in my first ten years of practice I didn’t help anyone get rid of their fungal nail infection as we were totally limited in what we could do. Our options were either ask the GP to prescribe systemic meds or asking the patient to apply antifungal topic treatments.
I’ve seen patients that have tried everything and categorically what has worked the best is the Lunula laser. It doesn’t have side effects, it is painless (the biggest plus point), research done on it has been incredibly effective and I have treated thousands of patients where almost every patient has had an improvement in their nails. We haven’t always had complete success in all of these cases, but we do work hard to achieve success for all our patients and we do get there almost 100% of the time. I run a business that uses Lunula solely for fungal nail infections, I don’t use anything else, I think that speaks for itself. Having used it for six and a half years, we’ve had great success with very happy patients.
To watch the complete webinar, head to:
For any questions or to learn more about how the Lunula laser can help your practice contact us:
Phone: 1300 653 522
Product Link: Click Here
Email: info@rehacare.co.nz